Caution:-
Ponstan (Mefenamic Acid) contains a warning:-
Caution should be exercised when treating patients suffering from epilepsy.
At lower doses Ponstan is antiepileptic, but at high doses it can have the opposite effect. This effect depends on the biological origin of the seizures.
In an earlier
post I wrote about a paper by Knut Wittkowski who applied statistics to
interpret the existing genetic data on autism.
“Autism treatments proposed by clinical studies and human genetics are complementary” & the NSAID Ponstan as a Novel AutismTherapy
His analysis
suggested the early use of Fenamate drugs could potentially reduce the
neurological anomalies that develop in autism as the brain develops. The natural question arose in the comments was
to whether it is too late to use Fenamates in later life.
Knut was
particularly looking at a handful of commonly affected genes (ANO 2/4/7 & KCNMA1) where defects should
partially be remedied by use of fenamates.
I recently received a comment
from a South African reader who finds that his children’s autism improves when
he gives them Ponstan and he wondered why.
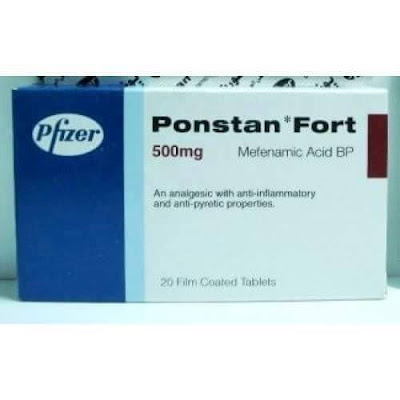
Ponstan (Mefenamic Acid) is a fenamate drug often used in many countries
as a pain killer, particularly in young children.
Ponstan is a cheap NSAID-type
drug very widely used in some countries and very rarely used in other countries
like the US. It is available without
prescription in some English-speaking countries (try a pharmacy in New Zealand,
who sell online) and, as Petra has pointed out, it is widely available in
Greece.
I did some more digging and was
surprised what other potentially very relevant effects Ponstan has. Ponstan affects GABAA receptors,
where it is a positive allosteric modulator (PAM). This may be very relevant to many people with
autism because we have seen that fine-tuning the response of the sub-units that
comprise GABAA receptors you can potentially improve cognition and
also modulate anxiety.
Anxiety
seems to be a core issue in Asperger’s, whereas in Classic Autism, or Strict
Definition Autism (SDA) the core issue is often actually cognitive function
rather than “autism” as such.
In this post
I will bring together the science showing why Ponstan should indeed be helpful
in some types of autism.
Professor
Ritvo from UCLA read Knut’s paper and also the bumetanide research and
suggested that babies could be treated with Ponstan and then, later on,
with Bumetanide.
Autism treatments proposed by clinical studies and human genetics are complementary
I do not
think the professor or Knut are aware of Ponstan’s effect on GABA.
The benefits
from Ponstan may very well be greater if given to babies at risk of autism, but
there does seem to be potential benefit for older children and adults, depending
on their type of autism.
Professor
Ritvo points out that that Ponstan is safely used in 6 month old babies, so
trialing it in children and adults with autism should not be troubling.
Being an
NSAID, long term use at high doses may well cause GI side effects. An open question is the dosage at which
Ponstan modulates the calcium activated ion channels that are implicated in some
autism and also what dosage affects GABAA receptors. It might well be lower than that required for
Ponstan’s known ant-inflammatory effects.
Ponstan vs Ibuprofen
Ibuprofen is
quite widely used in autism. Ibuprofen
is an NSAID but also a PPAR gamma agonist.
Ponstan is an NSAID but has no effect on PPAR gamma.
Research
shows that some types of autism respond to PPAR gamma agonists.
So it is
worth trying both Ponstan and Ibuprofen, but for somewhat different reasons.
They are
both interesting to deal with autism flare-ups, which seem common.
Other drugs
that people use short term, but are used long term in asthma therapy, are Singulair (Montelukast) and an
interesting Japanese drug called Ibudilast.
Singulair is a Western drug for maintenance therapy in asthma. Ibudilast is widely used in Japan as maintenance
therapy in Asthma, but works in a different way. Ibudilast is being used in clinical trials in
the US to treat Multiple Sclerosis.
Singulair is cheap and widely available, Ibudilast is more expensive and
available mainly in Japan.
Pre-vaccination Immunomodulation
In spite of
there being no publicly acknowledged link between vaccinations and autism
secondary to mitochondrial disease (AMD), I read that short term
immunomodulation is used prior to vaccination at Johns Hopkins, for some babies.
Singulair is
used, as is apparently ibuprofen.
Ponstan and Ibudilast would also likely be protective. Ponstan might well be the best choice; it
lowers fevers better than ibuprofen.
For those
open minded people, here is what a former head of the US National Institutes of Health, Bernadine Healy, had to say
about the safe vaccination. Not
surprisingly she was another Johns Hopkins trained doctor, as is Hannah Poling’s
Neurologist father.
The Vaccines-Autism War: Détente Needed
“Finally,
are certain groups of people especially susceptible to side effects from
vaccines, and can we identify them? Youngsters like Hannah Poling, for example,
who has an underlying mitochondrial disorder and developed a sudden and
dramatic case of regressive autism after receiving nine immunizations, later
determined to be the precipitating factor. Other children may have a genetic
predisposition to autism, a pre-existing neurological condition worsened by
vaccines, or an immune system that is sent into overdrive by too many vaccines,
and thus they might deserve special care. This approach challenges the notion
that every child must be vaccinated for every pathogen on the government's
schedule with almost no exception, a policy that means some will be sacrificed
so the vast majority benefit.”
So if I was an
American running the FDA/CDC I would suggest giving parents the option of
paying a couple of dollars for 10 days of Ponstan prior to these megadose
vaccinations and a few days afterwards.
No harm or good done in 99.9% of cases, but maybe some good done for the
remainder.
The fact the fact that nobody paid any attention to the late Dr Healy on this subject tells you a lot.
Fenamates (ANO 2/4/7 & KCNMA1)
Here Knut is
trying to target the ion channels expressed by the genes ANO 2/4/7 &
KCNMA1.
· KCNMA1 is a calcium activated
potassium channel. KCNMA1encodes the
ion channel KCa1.1, otherwise
known as BK (big potassium). This was the subject of post that I never
got round to publishing.
Fenamates are an
important group of clinically used non-steroidal anti-inflammatory drugs
(NSAIDs), but they have other effects beyond being anti-inflammatory.
They act as CaCC inhibitors and also stimulate
BKCa channel activity.
But fenamates also have a potent effect on what seems to be the most dysfunctional receptor in classic autism, the GABAA receptor.
The fenamate NSAID, mefenamic acid (MFA) prevents convulsions
and protects rats from seizure-induced forebrain damage evoked by pilocarpine
(Ikonomidou-Turski et al., 1988) and is anti-epileptogenic against
pentylenetetrazol (PTZ)-induced seizure activity, but at high doses induces seizures
(Wallenstein, 1991). In humans, MFA overdose can lead to convulsions and coma
(Balali-Mood et al, 1981; Young et al., 1979; Smolinske et al., 1990). More
recent data by Chen and colleagues (1998) have shown that the fenamates,
flufenamic, meclofenamic and mefenamic acid, protect chick embryo retinal
neurons against ischaemic and excitotoxic (kainate and NMDA) induced neuronal
cell death in vitro (Chen et al., 1998a; 1998b). MFA has also been reported to
reduce neuronal damage induced by intraventricular amyloid beta peptide
(Aβ1-42) and improve learning in rats treated with Aβ1-42 (Joo et al., 2006).
The mechanisms underlying these anti-epileptic and neuroprotective effects are
not well understood but together suggest that fenamates may influence neuronal
excitability through modulation of ligand and/or voltage-gated ion channels. In
the present study, therefore, we have investigated this hypothesis by
determining the actions of five representative fenamate NSAIDs at the major
excitatory and inhibitory ligand-gated ion channels in cultured hippocampal
neurons
This study demonstrates for the first time that mefenamic
acid and 4 other representatives of the fenamate NSAIDs are highly effective
and potent modulators of native hippocampal neuron GABAA receptors. MFA was the
most potent and at concentrations equal to or greater than 10 μM was also able
to directly activate the GABAA gated chloride channel. A previous study from
this laboratory reported that mefenamic acid potentiated recombinant GABAA receptors
expressed in HEK-293 cells and in Xenopus laevis oocytes (Halliwell et al.,
1999). Together these studies
lead to the conclusion that fenamate NSAIDs should now also be considered a
robust class of GABAA receptor modulators.
Also demonstrated for the first time here is the direct
activation of neuronal GABAA receptors by mefenamic acid. Other allosteric
potentiators, including the neuroactive steroids and the depressant
barbiturates share this property, with MFA at least equipotent to neurosteroids
and significantly more potent than the barbiturates. The mechanism(s) of the
direct gating of GABAA receptor chloride channels by MFA requires further
investigation using ultra-fast perfusion techniques but may be distinct from
that reported for neurosteroids (see, Hosie et al., 2006). Mefenamic acid
induced a leftward shift in the GABA dose-response curve consistent with an
increase in receptor affinity for the agonist. This is an action observed with
other positive allosteric GABAA receptor modulators, including the
benzodiazepine agonist, diazepam, the neuroactive steroid, allopregnanolone,
and the intravenous anesthetics, pentobarbitone and propofol (e.g. Johnston,
2005). To our knowledge, a unique property of MFA was that it was significantly
(F = 10.35; p≤ 0.001) more effective potentiating GABA currents at
hyperpolarized holding potentials (especially greater than −60mV). Further
experiments are required however to determine the underlying mechanism(s).
The highly effective modulation of GABAA receptors in
cultured hippocampal neurons suggests the fenamates may have central actions.
Consistent with this hypothesis, mefenamic acid concentrations are 40–80μM in
plasma with therapeutic doses (Cryer & Feldman, 1998); fenamates can also
cross the blood brain barrier (Houin et al., 1983; Bannwarth et al., 1989)
Coyne et al. Page 5 Neurochem Int. Author manuscript; available in PMC 2008
November 1. NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author
Manuscript and in overdose in humans are associated with coma and convulsions
(Smolinske et al., 1990). In animal studies, mefenamic acid is anticonvulsant
and neuroprotective against seizureinduced forebrain damage in rodents
(Ikonomidou-Turski et al., 1988). The present study would suggest that the anticonvulsant effects of
fenamates may be related, in part, to their efficacy to potentiate native GABAA
receptors in the brain, although a recent study has suggested that activation
of M-type K+ channels may contribute to this action (Peretz et al., 2005) Finally,
Joo and co-workers (2006) have recently reported that mefenamic acid provided
neuroprotection against β-amyloid (Aβ1-42) induced neurodegeneration and
attenuated cognitive impairments in this animal model of Alzheimer’s disease.
The authors proposed that neuroprotection may have resulted from inhibition of
cytochrome c release from mitochondria and reduced caspase-3 activation by
mefenamic acid. Clearly it would also be of interest to evaluate the role of
GABA receptor modulation in this in vivo model of Alzheimer’s disease.
Moreover, considerable evidence has emerged in the last few years indicating
that GABA receptor subtypes are involved in distinct neuronal functions and
subtype modulators may provide novel pharmacological therapies (Rudolf &
Mohler, 2006). Our present
data showing that fenamates are highly effective modulators of native GABAA
receptors and that mefenamic acid is highly subtype-selective (Halliwell et
al., 1999) suggests that further studies of its cognitive and behavioral
effects would be of value.
Note in the
above paper that NSAIDs other than mefenamic acid also modulate GABAA
receptors.
Just a
couple of months ago a rather complicated paper was published, again showing
that NSAIDs modulate GABAA receptors and showing that this is achieved
via the same calcium activated chloride channels (CaCC) referred to by Knut.
NSAIDs modulate GABA-activated currents via Ca2+-activated Cl− channels in rat dorsal root ganglion neurons
"Schematic displaying the effects
of CaCCs on GABA-activated inward currents and depolarization. GABA activates
the GABAA receptor to
open the Cl − channel
and the Cl− efflux
induces the depolarization response (inward current) of the membrane of dorsal
root ganglion (DRG) neurons. Then, voltage dependent L-type Ca2+ channels are activated by the depolarization,
and give rise to an increase in intracellular Ca2+. CaCCs are
activated by an increase in intracellular Ca2+ concentration which, in turn,
increases the driving force for Cl− efflux. Finally, the synergistic
action of the chloride ion efflux through GABAA receptors and NFA-sensitive CaCCs
causes GABA-activated currents or depolarization response in rat DRG neurons."
Note in the
complex explanation above the L-type calcium channels, which are already being
targeted by Verapamil, in the PolyPill.
Mefenamic Acid and Potassium Channels
We know that
Mefenamic acid also affects Kv7.1 (KvLQT1).
A closely
related substance called meclofenamic acid is known to act as novel KCNQ2/Q3
channel openers and is seen as having potential for the treatment of neuronal
hyper-excitability including epilepsy, migraine, or neuropathic pain.
The voltage-dependent M-type potassium current (M-current)
plays a major role in controlling brain excitability by stabilizing the
membrane potential and acting as a brake for neuronal firing. The KCNQ2/Q3
heteromeric channel complex was identified as the molecular correlate of the
M-current. Furthermore, the KCNQ2 and KCNQ3 channel subunits are mutated in families with benign
familial neonatal convulsions, a neonatal form of epilepsy. Enhancement of
KCNQ2/Q3 potassium currents may provide an important target for antiepileptic
drug development. Here, we show that meclofenamic acid (meclofenamate) and
diclofenac, two related molecules previously used as anti-inflammatory drugs,
act as novel KCNQ2/Q3 channel openers. Extracellular application of
meclofenamate (EC50 25 M) and diclofenac
(EC50 2.6 M) resulted in the activation
of KCNQ2/Q3 K currents, heterologously expressed in Chinese hamster ovary
cells. Both openers activated KCNQ2/Q3 channels by causing a hyperpolarizing
shift of the voltage activation curve (23 and 15 mV, respectively) and by
markedly slowing the deactivation kinetics. The effects of the drugs were
stronger on KCNQ2 than on KCNQ3 channel
subunits. In contrast, they did not enhance KCNQ1 K currents. Both
openers increased KCNQ2/Q3 current amplitude at physiologically relevant
potentials and led to hyperpolarization of the resting membrane potential. In
cultured cortical neurons, meclofenamate and diclofenac enhanced the M-current
and reduced evoked and spontaneous action potentials, whereas in vivo
diclofenac exhibited an anticonvulsant activity (ED50 43 mg/kg). These compounds potentially
constitute novel drug templates for the treatment of neuronal hyperexcitability
including epilepsy, migraine, or neuropathic pain. Volt
BK channel
KCNMA1encodes
the ion channel KCa1.1, otherwise
known as BK (big potassium). BK channels are implicated not only by Knut’s
statistics, but numerous studies ranging from schizophrenia to Fragile X.
Usually it is a case of too little BK channel activity.
The BK
channel is implicated in some epilepsy.
Pharmacology
BK channels are
pharmacological targets for the treatment of several medical disorders
including stroke and overactive bladder. Although pharmaceutical companies have attempted to develop
synthetic molecules targeting BK channels, their efforts have proved largely ineffective. For instance,
BMS-204352, a molecule developed by Bristol-Myers Squibb, failed to improve clinical outcome in stroke patients compared
to placebo. However, BKCa channels are reduced in patients suffering from
the Fragile X syndrome and the agonist, BMS-204352, corrects some of the deficits
observed in Fmr1 knockout
mice, a model of Fragile X syndrome.
BK channels have also
been found to be activated by exogenous pollutants and endogenous gasotransmitters carbon monoxide and hydrogen sulphide.
BK channels can be
readily inhibited by a range of compounds including tetraethylammonium (TEA), paxilline and iberiotoxin.
Achieving a better understanding
of BK channel function is important not only for furthering our knowledge of
the involvement of these channels in physiological processes, but also for
pathophysiological conditions, as has been demonstrated by recent discoveries
implicating these channels in neurological disorders. One such disorder is
schizophrenia where BK channels are hypothesized to play a role in the etiology
of the disease due to the effects of commonly used antipsychotic drugs on
enhancing K+ conductance [101]. Furthermore, this
same study found that the mRNA expression levels of the BK channel were
significantly lower in the prefrontal cortex of the schizophrenic group than in
the control group [101]. Similarly, autism and mental retardation have been
linked to haploinsufficiency of the Slo1 gene and decreased BK channel expression [102].
Two mutations in BK channel genes have been associated
with epilepsy. One mutation has been identified on the accessory β3 subunit,
which results in an early truncation of the protein and has been significantly
correlated in patients with idiopathic generalized epilepsy [103]. The other mutation
is located on the Slo1gene, and was
identified through genetic screening of a family with generalized epilepsy and
paroxysmal dyskinesia [104]. The biophysical
properties of this Slo1 mutation indicates enhanced sensitivity to Ca2+ and an increased average time that the channel remains
open [104–107]. This increased Ca2+ sensitivity is dependent on the specific type of β
subunit associating with the BK channel [106, 107]. In association
with the β3 subunit, the mutation does not alter the Ca2+-dependent
properties of the channel, but with the β4 subunit the mutation increases the
Ca2+ sensitivity [105–107]. This is
significant considering the relatively high abundance of the β4 subunit
compared to the weak distribution of the β3 subunit in the brain [12, 13,15, 106, 107]. It has been
proposed that a gain of BK channel function may result in increases in the
firing frequency due to rapid repolarization of APs, which allows a quick
recovery of Na+ channels from
inactivation, thereby facilitating the firing of subsequent APs [104]. Supporting this
hypothesis, mice null for the β4 subunit showed enhanced Ca2+ sensitivity of BK channels, resulting in temporal lobe
epilepsy, which was likely due to a shortened duration and increased frequency
of APs [108]. An interesting
relevance to the mechanisms of BK channel activation as discussed above, the
Slo1 mutation associated with epilepsy only alters Ca2+ dependent activation originated from the Ca2+ binding site in RCK1, but not from the Ca2+bowl,
by altering the coupling mechanism between Ca2+ binding and gate opening [100]. Since Ca2+dependent
activation originated from the Ca2+ binding site in RCK1 is enhanced by membrane
depolarization, at the peak of an action potential the binding of Ca2+ to the site in RCK1 contributes much more than binding
to the Ca2+ bowl to activating
the channel [84, 109].
Although these associations
between specific mutations in BK channel subunits and various neurological
disorders have been demonstrated by numerous studies, it is also important to
point out certain caveats with these studies, such as genetic linkage between
BK channels and different diseases do not necessary show causation as these
studies were performed based on correlation between changes in the
protein/genetic marker and overall phenotype. Furthermore, studies performed
using a mouse model also can fail to indicate what may happen in higher-order
species, and this is especially true for BK channels, where certain β subunits
are only primate specific [110].
Possible role of potassium channel, big K in etiology of schizophrenia.
Schizophrenia (SZ), a common severe mental disorder, affecting about 1% of the world population. However, the etiology of SZ is still largely unknown. It is believed that molecules that are in an association with the etiology and pathology of SZ are neurotransmitters including dopamine, 5-HT and gamma-aminobutyric acid (GABA). But several lines of evidences indicate that potassium large conductance calcium-activated channel, known as BK channel, is likely to be included. BK channel belongs to a group of ion channels that plays an important role in regulating neuronal excitability and transmitter releasing. Its involvement in SZ emerges as a great interest. For example, commonly used neuroleptics, in clinical therapeutic concentrations, alter calcium-activated potassium conductance in central neurons. Diazoxide, a potassium channel opener/activator, showed a significant superiority over haloperidol alone in the treatment of positive and general psychopathology symptoms in SZ. Additionally, estrogen, which regulates the activity of BK channel, modulates dopaminergic D2 receptor and has an antipsychotic-like effect. Therefore, we hypothesize that BK channel may play a role in SZ and those agents, which can target either BK channel functions or its expression may contribute to the therapeutic actions of SZ treatment.
Conclusion
It appears
that Ponstan and related substances have some interesting effects that are only now
emerging in the research.
People with
autism, and indeed schizophrenia, may potentially benefit from Ponstan and for a variety of different reasons.
I think it
will take many decades for any conclusive research to be published on this
subject, because this is an off-patent generic drug.
As with most
NSAIDS, it is simple to trial Ponstan.