Caution:-
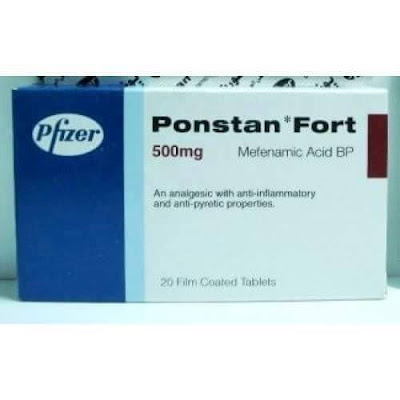
Ponstan (Mefenamic Acid) contains a warning:-
Caution should be exercised when treating patients suffering from epilepsy.
At lower doses Ponstan is antiepileptic, but at high doses it can have the opposite effect. This effect depends on the biological origin of the seizures.
In an earlier
post I wrote about a paper by Knut Wittkowski who applied statistics to
interpret the existing genetic data on autism.
“Autism treatments proposed by clinical studies and human genetics are complementary” & the NSAID Ponstan as a Novel AutismTherapy
His analysis
suggested the early use of Fenamate drugs could potentially reduce the
neurological anomalies that develop in autism as the brain develops. The natural question arose in the comments was
to whether it is too late to use Fenamates in later life.
Knut was
particularly looking at a handful of commonly affected genes (ANO 2/4/7 & KCNMA1) where defects should
partially be remedied by use of fenamates.
I recently received a comment
from a South African reader who finds that his children’s autism improves when
he gives them Ponstan and he wondered why.
Ponstan (Mefenamic Acid) is a fenamate drug often used in many countries
as a pain killer, particularly in young children.
Ponstan is a cheap NSAID-type
drug very widely used in some countries and very rarely used in other countries
like the US. It is available without
prescription in some English-speaking countries (try a pharmacy in New Zealand,
who sell online) and, as Petra has pointed out, it is widely available in
Greece.
I did some more digging and was
surprised what other potentially very relevant effects Ponstan has. Ponstan affects GABAA receptors,
where it is a positive allosteric modulator (PAM). This may be very relevant to many people with
autism because we have seen that fine-tuning the response of the sub-units that
comprise GABAA receptors you can potentially improve cognition and
also modulate anxiety.
Anxiety
seems to be a core issue in Asperger’s, whereas in Classic Autism, or Strict
Definition Autism (SDA) the core issue is often actually cognitive function
rather than “autism” as such.
In this post
I will bring together the science showing why Ponstan should indeed be helpful
in some types of autism.
Professor
Ritvo from UCLA read Knut’s paper and also the bumetanide research and
suggested that babies could be treated with Ponstan and then, later on,
with Bumetanide.
Autism treatments proposed by clinical studies and human genetics are complementary
I do not
think the professor or Knut are aware of Ponstan’s effect on GABA.
The benefits
from Ponstan may very well be greater if given to babies at risk of autism, but
there does seem to be potential benefit for older children and adults, depending
on their type of autism.
Professor
Ritvo points out that that Ponstan is safely used in 6 month old babies, so
trialing it in children and adults with autism should not be troubling.
Being an
NSAID, long term use at high doses may well cause GI side effects. An open question is the dosage at which
Ponstan modulates the calcium activated ion channels that are implicated in some
autism and also what dosage affects GABAA receptors. It might well be lower than that required for
Ponstan’s known ant-inflammatory effects.
Ponstan vs Ibuprofen
Ibuprofen is
quite widely used in autism. Ibuprofen
is an NSAID but also a PPAR gamma agonist.
Ponstan is an NSAID but has no effect on PPAR gamma.
Research
shows that some types of autism respond to PPAR gamma agonists.
So it is
worth trying both Ponstan and Ibuprofen, but for somewhat different reasons.
They are
both interesting to deal with autism flare-ups, which seem common.
Other drugs
that people use short term, but are used long term in asthma therapy, are Singulair (Montelukast) and an
interesting Japanese drug called Ibudilast.
Singulair is a Western drug for maintenance therapy in asthma. Ibudilast is widely used in Japan as maintenance
therapy in Asthma, but works in a different way. Ibudilast is being used in clinical trials in
the US to treat Multiple Sclerosis.
Singulair is cheap and widely available, Ibudilast is more expensive and
available mainly in Japan.
Pre-vaccination Immunomodulation
In spite of
there being no publicly acknowledged link between vaccinations and autism
secondary to mitochondrial disease (AMD), I read that short term
immunomodulation is used prior to vaccination at Johns Hopkins, for some babies.
Singulair is
used, as is apparently ibuprofen.
Ponstan and Ibudilast would also likely be protective. Ponstan might well be the best choice; it
lowers fevers better than ibuprofen.
For those
open minded people, here is what a former head of the US National Institutes of Health, Bernadine Healy, had to say
about the safe vaccination. Not
surprisingly she was another Johns Hopkins trained doctor, as is Hannah Poling’s
Neurologist father.
The Vaccines-Autism War: Détente Needed
“Finally,
are certain groups of people especially susceptible to side effects from
vaccines, and can we identify them? Youngsters like Hannah Poling, for example,
who has an underlying mitochondrial disorder and developed a sudden and
dramatic case of regressive autism after receiving nine immunizations, later
determined to be the precipitating factor. Other children may have a genetic
predisposition to autism, a pre-existing neurological condition worsened by
vaccines, or an immune system that is sent into overdrive by too many vaccines,
and thus they might deserve special care. This approach challenges the notion
that every child must be vaccinated for every pathogen on the government's
schedule with almost no exception, a policy that means some will be sacrificed
so the vast majority benefit.”
So if I was an
American running the FDA/CDC I would suggest giving parents the option of
paying a couple of dollars for 10 days of Ponstan prior to these megadose
vaccinations and a few days afterwards.
No harm or good done in 99.9% of cases, but maybe some good done for the
remainder.
The fact the fact that nobody paid any attention to the late Dr Healy on this subject tells you a lot.
Fenamates (ANO 2/4/7 & KCNMA1)
Here Knut is
trying to target the ion channels expressed by the genes ANO 2/4/7 &
KCNMA1.
· KCNMA1 is a calcium activated
potassium channel. KCNMA1encodes the
ion channel KCa1.1, otherwise
known as BK (big potassium). This was the subject of post that I never
got round to publishing.
Fenamates are an
important group of clinically used non-steroidal anti-inflammatory drugs
(NSAIDs), but they have other effects beyond being anti-inflammatory.
They act as CaCC inhibitors and also stimulate
BKCa channel activity.
But fenamates also have a potent effect on what seems to be the most dysfunctional receptor in classic autism, the GABAA receptor.
The fenamate NSAID, mefenamic acid (MFA) prevents convulsions
and protects rats from seizure-induced forebrain damage evoked by pilocarpine
(Ikonomidou-Turski et al., 1988) and is anti-epileptogenic against
pentylenetetrazol (PTZ)-induced seizure activity, but at high doses induces seizures
(Wallenstein, 1991). In humans, MFA overdose can lead to convulsions and coma
(Balali-Mood et al, 1981; Young et al., 1979; Smolinske et al., 1990). More
recent data by Chen and colleagues (1998) have shown that the fenamates,
flufenamic, meclofenamic and mefenamic acid, protect chick embryo retinal
neurons against ischaemic and excitotoxic (kainate and NMDA) induced neuronal
cell death in vitro (Chen et al., 1998a; 1998b). MFA has also been reported to
reduce neuronal damage induced by intraventricular amyloid beta peptide
(Aβ1-42) and improve learning in rats treated with Aβ1-42 (Joo et al., 2006).
The mechanisms underlying these anti-epileptic and neuroprotective effects are
not well understood but together suggest that fenamates may influence neuronal
excitability through modulation of ligand and/or voltage-gated ion channels. In
the present study, therefore, we have investigated this hypothesis by
determining the actions of five representative fenamate NSAIDs at the major
excitatory and inhibitory ligand-gated ion channels in cultured hippocampal
neurons
This study demonstrates for the first time that mefenamic
acid and 4 other representatives of the fenamate NSAIDs are highly effective
and potent modulators of native hippocampal neuron GABAA receptors. MFA was the
most potent and at concentrations equal to or greater than 10 μM was also able
to directly activate the GABAA gated chloride channel. A previous study from
this laboratory reported that mefenamic acid potentiated recombinant GABAA receptors
expressed in HEK-293 cells and in Xenopus laevis oocytes (Halliwell et al.,
1999). Together these studies
lead to the conclusion that fenamate NSAIDs should now also be considered a
robust class of GABAA receptor modulators.
Also demonstrated for the first time here is the direct
activation of neuronal GABAA receptors by mefenamic acid. Other allosteric
potentiators, including the neuroactive steroids and the depressant
barbiturates share this property, with MFA at least equipotent to neurosteroids
and significantly more potent than the barbiturates. The mechanism(s) of the
direct gating of GABAA receptor chloride channels by MFA requires further
investigation using ultra-fast perfusion techniques but may be distinct from
that reported for neurosteroids (see, Hosie et al., 2006). Mefenamic acid
induced a leftward shift in the GABA dose-response curve consistent with an
increase in receptor affinity for the agonist. This is an action observed with
other positive allosteric GABAA receptor modulators, including the
benzodiazepine agonist, diazepam, the neuroactive steroid, allopregnanolone,
and the intravenous anesthetics, pentobarbitone and propofol (e.g. Johnston,
2005). To our knowledge, a unique property of MFA was that it was significantly
(F = 10.35; p≤ 0.001) more effective potentiating GABA currents at
hyperpolarized holding potentials (especially greater than −60mV). Further
experiments are required however to determine the underlying mechanism(s).
The highly effective modulation of GABAA receptors in
cultured hippocampal neurons suggests the fenamates may have central actions.
Consistent with this hypothesis, mefenamic acid concentrations are 40–80μM in
plasma with therapeutic doses (Cryer & Feldman, 1998); fenamates can also
cross the blood brain barrier (Houin et al., 1983; Bannwarth et al., 1989)
Coyne et al. Page 5 Neurochem Int. Author manuscript; available in PMC 2008
November 1. NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author
Manuscript and in overdose in humans are associated with coma and convulsions
(Smolinske et al., 1990). In animal studies, mefenamic acid is anticonvulsant
and neuroprotective against seizureinduced forebrain damage in rodents
(Ikonomidou-Turski et al., 1988). The present study would suggest that the anticonvulsant effects of
fenamates may be related, in part, to their efficacy to potentiate native GABAA
receptors in the brain, although a recent study has suggested that activation
of M-type K+ channels may contribute to this action (Peretz et al., 2005) Finally,
Joo and co-workers (2006) have recently reported that mefenamic acid provided
neuroprotection against β-amyloid (Aβ1-42) induced neurodegeneration and
attenuated cognitive impairments in this animal model of Alzheimer’s disease.
The authors proposed that neuroprotection may have resulted from inhibition of
cytochrome c release from mitochondria and reduced caspase-3 activation by
mefenamic acid. Clearly it would also be of interest to evaluate the role of
GABA receptor modulation in this in vivo model of Alzheimer’s disease.
Moreover, considerable evidence has emerged in the last few years indicating
that GABA receptor subtypes are involved in distinct neuronal functions and
subtype modulators may provide novel pharmacological therapies (Rudolf &
Mohler, 2006). Our present
data showing that fenamates are highly effective modulators of native GABAA
receptors and that mefenamic acid is highly subtype-selective (Halliwell et
al., 1999) suggests that further studies of its cognitive and behavioral
effects would be of value.
Note in the
above paper that NSAIDs other than mefenamic acid also modulate GABAA
receptors.
Just a
couple of months ago a rather complicated paper was published, again showing
that NSAIDs modulate GABAA receptors and showing that this is achieved
via the same calcium activated chloride channels (CaCC) referred to by Knut.
NSAIDs modulate GABA-activated currents via Ca2+-activated Cl− channels in rat dorsal root ganglion neurons
"Schematic displaying the effects
of CaCCs on GABA-activated inward currents and depolarization. GABA activates
the GABAA receptor to
open the Cl − channel
and the Cl− efflux
induces the depolarization response (inward current) of the membrane of dorsal
root ganglion (DRG) neurons. Then, voltage dependent L-type Ca2+ channels are activated by the depolarization,
and give rise to an increase in intracellular Ca2+. CaCCs are
activated by an increase in intracellular Ca2+ concentration which, in turn,
increases the driving force for Cl− efflux. Finally, the synergistic
action of the chloride ion efflux through GABAA receptors and NFA-sensitive CaCCs
causes GABA-activated currents or depolarization response in rat DRG neurons."
Note in the
complex explanation above the L-type calcium channels, which are already being
targeted by Verapamil, in the PolyPill.
Mefenamic Acid and Potassium Channels
We know that
Mefenamic acid also affects Kv7.1 (KvLQT1).
A closely
related substance called meclofenamic acid is known to act as novel KCNQ2/Q3
channel openers and is seen as having potential for the treatment of neuronal
hyper-excitability including epilepsy, migraine, or neuropathic pain.
The voltage-dependent M-type potassium current (M-current)
plays a major role in controlling brain excitability by stabilizing the
membrane potential and acting as a brake for neuronal firing. The KCNQ2/Q3
heteromeric channel complex was identified as the molecular correlate of the
M-current. Furthermore, the KCNQ2 and KCNQ3 channel subunits are mutated in families with benign
familial neonatal convulsions, a neonatal form of epilepsy. Enhancement of
KCNQ2/Q3 potassium currents may provide an important target for antiepileptic
drug development. Here, we show that meclofenamic acid (meclofenamate) and
diclofenac, two related molecules previously used as anti-inflammatory drugs,
act as novel KCNQ2/Q3 channel openers. Extracellular application of
meclofenamate (EC50 25 M) and diclofenac
(EC50 2.6 M) resulted in the activation
of KCNQ2/Q3 K currents, heterologously expressed in Chinese hamster ovary
cells. Both openers activated KCNQ2/Q3 channels by causing a hyperpolarizing
shift of the voltage activation curve (23 and 15 mV, respectively) and by
markedly slowing the deactivation kinetics. The effects of the drugs were
stronger on KCNQ2 than on KCNQ3 channel
subunits. In contrast, they did not enhance KCNQ1 K currents. Both
openers increased KCNQ2/Q3 current amplitude at physiologically relevant
potentials and led to hyperpolarization of the resting membrane potential. In
cultured cortical neurons, meclofenamate and diclofenac enhanced the M-current
and reduced evoked and spontaneous action potentials, whereas in vivo
diclofenac exhibited an anticonvulsant activity (ED50 43 mg/kg). These compounds potentially
constitute novel drug templates for the treatment of neuronal hyperexcitability
including epilepsy, migraine, or neuropathic pain. Volt
BK channel
KCNMA1encodes
the ion channel KCa1.1, otherwise
known as BK (big potassium). BK channels are implicated not only by Knut’s
statistics, but numerous studies ranging from schizophrenia to Fragile X.
Usually it is a case of too little BK channel activity.
The BK
channel is implicated in some epilepsy.
Pharmacology
BK channels are
pharmacological targets for the treatment of several medical disorders
including stroke and overactive bladder. Although pharmaceutical companies have attempted to develop
synthetic molecules targeting BK channels, their efforts have proved largely ineffective. For instance,
BMS-204352, a molecule developed by Bristol-Myers Squibb, failed to improve clinical outcome in stroke patients compared
to placebo. However, BKCa channels are reduced in patients suffering from
the Fragile X syndrome and the agonist, BMS-204352, corrects some of the deficits
observed in Fmr1 knockout
mice, a model of Fragile X syndrome.
BK channels have also
been found to be activated by exogenous pollutants and endogenous gasotransmitters carbon monoxide and hydrogen sulphide.
BK channels can be
readily inhibited by a range of compounds including tetraethylammonium (TEA), paxilline and iberiotoxin.
Achieving a better understanding
of BK channel function is important not only for furthering our knowledge of
the involvement of these channels in physiological processes, but also for
pathophysiological conditions, as has been demonstrated by recent discoveries
implicating these channels in neurological disorders. One such disorder is
schizophrenia where BK channels are hypothesized to play a role in the etiology
of the disease due to the effects of commonly used antipsychotic drugs on
enhancing K+ conductance [101]. Furthermore, this
same study found that the mRNA expression levels of the BK channel were
significantly lower in the prefrontal cortex of the schizophrenic group than in
the control group [101]. Similarly, autism and mental retardation have been
linked to haploinsufficiency of the Slo1 gene and decreased BK channel expression [102].
Two mutations in BK channel genes have been associated
with epilepsy. One mutation has been identified on the accessory β3 subunit,
which results in an early truncation of the protein and has been significantly
correlated in patients with idiopathic generalized epilepsy [103]. The other mutation
is located on the Slo1gene, and was
identified through genetic screening of a family with generalized epilepsy and
paroxysmal dyskinesia [104]. The biophysical
properties of this Slo1 mutation indicates enhanced sensitivity to Ca2+ and an increased average time that the channel remains
open [104–107]. This increased Ca2+ sensitivity is dependent on the specific type of β
subunit associating with the BK channel [106, 107]. In association
with the β3 subunit, the mutation does not alter the Ca2+-dependent
properties of the channel, but with the β4 subunit the mutation increases the
Ca2+ sensitivity [105–107]. This is
significant considering the relatively high abundance of the β4 subunit
compared to the weak distribution of the β3 subunit in the brain [12, 13,15, 106, 107]. It has been
proposed that a gain of BK channel function may result in increases in the
firing frequency due to rapid repolarization of APs, which allows a quick
recovery of Na+ channels from
inactivation, thereby facilitating the firing of subsequent APs [104]. Supporting this
hypothesis, mice null for the β4 subunit showed enhanced Ca2+ sensitivity of BK channels, resulting in temporal lobe
epilepsy, which was likely due to a shortened duration and increased frequency
of APs [108]. An interesting
relevance to the mechanisms of BK channel activation as discussed above, the
Slo1 mutation associated with epilepsy only alters Ca2+ dependent activation originated from the Ca2+ binding site in RCK1, but not from the Ca2+bowl,
by altering the coupling mechanism between Ca2+ binding and gate opening [100]. Since Ca2+dependent
activation originated from the Ca2+ binding site in RCK1 is enhanced by membrane
depolarization, at the peak of an action potential the binding of Ca2+ to the site in RCK1 contributes much more than binding
to the Ca2+ bowl to activating
the channel [84, 109].
Although these associations
between specific mutations in BK channel subunits and various neurological
disorders have been demonstrated by numerous studies, it is also important to
point out certain caveats with these studies, such as genetic linkage between
BK channels and different diseases do not necessary show causation as these
studies were performed based on correlation between changes in the
protein/genetic marker and overall phenotype. Furthermore, studies performed
using a mouse model also can fail to indicate what may happen in higher-order
species, and this is especially true for BK channels, where certain β subunits
are only primate specific [110].
Possible role of potassium channel, big K in etiology of schizophrenia.
Schizophrenia (SZ), a common severe mental disorder, affecting about 1% of the world population. However, the etiology of SZ is still largely unknown. It is believed that molecules that are in an association with the etiology and pathology of SZ are neurotransmitters including dopamine, 5-HT and gamma-aminobutyric acid (GABA). But several lines of evidences indicate that potassium large conductance calcium-activated channel, known as BK channel, is likely to be included. BK channel belongs to a group of ion channels that plays an important role in regulating neuronal excitability and transmitter releasing. Its involvement in SZ emerges as a great interest. For example, commonly used neuroleptics, in clinical therapeutic concentrations, alter calcium-activated potassium conductance in central neurons. Diazoxide, a potassium channel opener/activator, showed a significant superiority over haloperidol alone in the treatment of positive and general psychopathology symptoms in SZ. Additionally, estrogen, which regulates the activity of BK channel, modulates dopaminergic D2 receptor and has an antipsychotic-like effect. Therefore, we hypothesize that BK channel may play a role in SZ and those agents, which can target either BK channel functions or its expression may contribute to the therapeutic actions of SZ treatment.
Conclusion
It appears
that Ponstan and related substances have some interesting effects that are only now
emerging in the research.
People with
autism, and indeed schizophrenia, may potentially benefit from Ponstan and for a variety of different reasons.
I think it
will take many decades for any conclusive research to be published on this
subject, because this is an off-patent generic drug.
As with most
NSAIDS, it is simple to trial Ponstan.

Interesting post Peter. To add more fuel to the fire here is an article I read today about another genomics study strongly linking autism to schizophrenia (which you discussed in length in this latest post of yours):
ReplyDeletehttps://spectrumnews.org/news/brain-tissue-study-bolsters-autism-schizophrenia-link/
Also, something else I came across which I believe downstream may be one small part in a comprehensive therapy for achieving acceptable outcomes for severely autistic people:
http://med.stanford.edu/news/all-news/2016/06/stem-cells-shown-safe-beneficial-for-chronic-stroke-patients.html
What this shows is that stem cell therapy is not only safe, but very beneficial to stroke victims. I have read quite a lot of about stroke and there are some striking similarities to autism in terms of the type of stress and the way the immune system reacts (or overreacts) at the cellular level. While stroke itself is acute (just like concussions from years of football playing) the recovery process and the cleanup/repair process can go awry and do more damage than good and lead to chronic brain encephalitis over time. This is an open debate in autism since having a big database of donated brain tissue from those with autism at all ages of life makes studies on the matter rather underpowered, but there does seem to be a trend in what I have read where children with autism have an overabundance of brain cells and then by the time they are adults, they show the kind of signs of stress you find in other degenerative brain diseases to the point you might look at a 30 year old brain of someone with autism and conclude that it looks like that of a 50 year old.
Hi Peter, Liquid food processing is different to solid food.
ReplyDeleteI'll start with a conclusion which may be incorrect, particularly when it comes to drugs. I'm sure you can check on that.
Ponstan treatment has really intrigued me since when you released your earlier relevant post.
I used Ponstan syrup for my son as a baby and during his childhood years, after vaccinations, when fever, inflammation etc., very effectively.
Going back to Ponstan pills as an adult I had mixed results and this has made me curious.
Possible reasonable explanations I've come up with is the fact that pills may cause GI side effects or processed differently or the dose is too high. I now see that Ponstan is not well tolerated with the evidence he definitely has GI isues.
It may be the syrup that works better for some responders. This might also apply to melatonin supplementation; I'll have to check.
Low dose Baclofen replaced both Ponstan and Ibuprofen when there is a "hidden" inlammation. According to my observations, some food, processed carbs in particular, affect my son. He gets agitated, serotonin drops and when given baclofen it really helps him.
It also ameliorates cholinergic function.
There are some papers supporting Baclofen alters gut to brain signaling during inflammation and also GABA B agonists (in rabbits) are dependent on cholinergic neurotransmission. It seems that it's not as harmful for GI as anti-inflamatory drugs should be.
So, if you find reason for liquid Postan, I could always send you from Greece, where it's widely available.
Test
ReplyDeleteThis comment has been removed by the author.
ReplyDeleteIn the UK prescribing is very much limited to what NICE (National Institute for Clinical Excellence) recommend. They made a very detailed review of the autism literature and concluded that nothing works. I trialled Bumetanide, which had been reviewed by NICE, and it certainly did work in our case.
DeleteThe three key drugs I use (Bumetanide, Verapamil and Atorvastatin) are all drugs used long term by many people 50+. As a result in countries like Spain these drugs are handed out by pharmacists without the need for a prescription, even though they are prescription drugs. This may sound odd to someone in Northern Europe. If you specifically ask do you need a prescription they would say yes.
In the US there are doctors who will prescribe off-label, i.e. for uses that are not specifically approved.
So if you want to treat autism you will have to self treat. This is frowned upon because some people will end up doing stupid things, but you can also do stupid things with supplements freely available on Amazon.
Many people use offshore internet pharmacies, it is probably cheaper to have a City break in Spain.
Thank you for your reply Peter. I will certainly do this. I wonder whether France or Ireland are the same...I will look into this also as easier for me to drive to these locations.
DeleteThe research you are doing is so valuable, It would be good to see this work acknowledged. Best of luck,
Kind regards
Sarah
Sarah, I know for sure that France, Germany, Austria, Poland all require a prescription. The only flexible countries are the more Latin ones. Greece is flexible, but do not have bumetanide. I think Ireland will be just like the UK. Some things are drugs, eg Ponstan, in the UK but OTC in other countries. Things like NAC are available on Amazon and similar sites. NAC is very helpful in many cases.
DeleteThank you Peter, I will go to Spain for sure. I did buy NAC from Amazon but like you detailed the sulphur odour happened pretty much as soon as the bag of powder was opened, I think the best way is to open the capsules, but again the dosage is harder to gauge when opening capsules. My son has started refusing to take tablets now (because he never swallows - always bites/chews - when I gave him a couple of other softgels recently he wasn't impressed with the taste so this has put him off) so the only way to get things into him is via liquid versions in juice.
DeleteOn another note I wanted to share the link on Dr Mary Newport which links cognition improvements to Coconut Oil (we have been using it over 8 weeks and it seems promising)
https://www.youtube.com/watch?v=feyydeMFWy4
kind regards
Sarah
Coconut oil and some other changes would take you towards a ketogenic diet, which does help some people, particularly those with epilepsy.
Deletemy son seems to have inflammatory pain reaction to coconut oil, coconut milk, MCT oil. Last check two yrs ago his cholesterol was high. Sticking with just olive oil.
ReplyDeleteHi Peter and all of you contributing with insightful comments!
ReplyDeleteYou have been a true resource for me during the worst time of my life when I realized my sweet daughter had autism and there was no cure...
I am now mentally ready to start some medical intervention for her.
My daughter is almost 2 years old and around 13 kg.
She seems to have classic autism, with impaired cognition, "slow", nonverbal, apraxic, but social.
No known allergies (small skin reaction to cinnamon though), no GI, no bad behaviour, no sleeping problems, no sensory overload. Yet.
I was pondering Bumetadin, but then saw the posts on Ponstan (still looking for information on dosage/length of treatment).
What else would you recommend as a starting point for medical intervention for someone as small (and still maybe having a window of opportunity)?
Also, maybe you could recommend any tests that she should do to get a better idea of what phenotype she belongs to? Genetic testing did not show anything special, and some metabolic tests were done as part of national PKU-testing with no result.
I am trying to get an EEG "just in case".
Thanks in advance,
/Ling
Ling, why not contact Knut Wittkowski, Rockefeller University, and ask him about Ponstan. It is his big idea.
DeleteThe suggestion either in this post, or another one from the clinician at UCLA was to start Ponstan and Bumetanide ASAP.
"Yet" is very relevant. Autism tends to get worse.
Antioxidants like NAC may be protective and prevent some damage.
Ling,
DeleteBumetanide (a very strong diuretic) blocks *in*flux of chloride into neurons. This decreases excitability only in children who fall not asleep with valium.
Mefenamic acid (an NSAID) blocks the *ef*flux of chlorid from neurons (and activates the efflux of potassium). Both actions should decrease excitability most >1 yr old children.
Unless your daughter has the above paradoxical response to valium, bumetanide and mefenamic acid may have opposite effects. You should discuss with your physician which drug might work best for your daughter.
The approved dose in the UK for Ponstan is 25 mg/kg/d in four divided doses, but to prevent mutism one would only need to give 6 mg/kg twice (morning and noon).
/Knut
Still confused about ponstan in that is it an alternative to bumetanide use and will have the same function as bumetanide or is it a different thing altogether
DeleteCheers Paul
A different thing altogether. Ponstan may help 1-yr olds with developing language, bumetanide has shown mixed results in older children.
DeleteKnut
This is a very late reply to the question "Is Ponstan (mefenamic acid) an alternative to Bumetanide?", but I think it is still relevant.
DeleteSince I am not a doctor I cannot put this in correct medical terms, but I think I can answer in words that are more comprehensible.
No, Ponstan is not comparable to Bumetanide, as they do not share any main pharmacological effects. They are not working on the same pathways (channels) and using them together is generally not recommended. This doesn't mean that they can't have the same medical effect of lifting cognition in different persons or even in the same person. It all depends on the individual dysfunctions that are present; genetic or autoimmune or something else.
But, Ponstan could to some extent be compared to Verapamil.
Verapamil blocks calcium influx into cells, it is a calcium channel blocker. In many autisms, there is a genetic dysfunction in these channels so that too much calcium flows into the cells. This is the very start of a long chain of processes that together with other dysfunctions on the way create that particular autism.
Calcium influx means that intracellular calcium levels rise. If this happens, some chloride channels are activated. If you use Verapamil, these chloride channels won't be activated since there is less calcium flowing in.
If you use Ponstan instead, you directly block activation of these chloride channels. Also, you activate a potassium channel that closes the calcium channels mentioned above. Both of these mechanisms are also implicated dysfunctional by genetic autism research.
So, depending on the present genetic dysfunctions (CACNA1x-family or ANO-family / KCNMA1) or immunological profile (at least we know there exists antibodies to ANO2) one of these medications might be the better choice. They have both other and highly relevant interactions, so the choice is not simple.
Sorry for repeating stuff in this blog already, but I think newcomers appreciate short summaries and I don’t want anyone to have to go through the research I had to do to put things together.
/Ling (hoping that Peter will correct me if I write stupidities!) :-)
Seems that taking the idea of mefenamic acid for autism to the treatment level just took a great step forward:
ReplyDeletehttp://medcitynews.com/2017/04/q-biomed-early-stage-autism-deal-asdera/?rf=1
/Ling
I am not sure if this adds anything to our knowledge regarding mefenamic acid/Ponstan, but I link to it since it seems relevant (I just don't know how yet ;-) ):
ReplyDeletehttp://www.tandfonline.com/doi/abs/10.3109/10715762.2012.669836?src=recsys&journalCode=ifra20
"We found that D-serine significantly increased oxidative stress, levels of inflammation- and apoptosis-related molecules in a region specific manner. Mefenamic acid treatment provided significant protection against the elevation of lipid peroxidation, protein oxidation, levels of TNF-α, IL-1β and Bax. "
/Ling
Finally, here is my report on 1 month use of mefenamic acid for autism (and pain).
ReplyDeleteMy daughter is 25 months / 13 kg. She had 80 mg Ponstan from a divided capsule twice a day. No interfering medication, but she was having a new tooth during the first weeks.
-----------------------------------
The first few days I noticed that she seemed faster, in everything. She was almost running around our house, when she usually toddles. Maybe it was something about faster reactions or better coordination? She also seemed “stronger”, suddenly using her muscles and squeezing me hard with her hands on a couple of occasions. The painkilling effect was very clear and superior to the usual paracetamol/acetaminophen.
At day ten I could see a strange pattern: two hours or so after intake she would lean forward and scream joyfully. I have no idea what this was about, but she sure seemed to enjoy it. Some irritability, which might or might not be related.
Around day 14 or so she started to notice details that she had not “seen” before. The most obvious example would be when she was pointing at the two paintings that have been hanging over her bed since she was born. Or, some knobs in eye-height on her drawer that she passes many times each day but never has been interested in.
Day 17. At this time I asked myself if her receptive language was better than before (or placebo effect on me). She would of course not understand so many new words after such a short period, but if something was messing with her neurological hearing capabilities before and now was inhibited it would surely look like this. She was also much more active – not hyperactive, but “normal” active for a 2 year old kid. No social gain yet.
Day 25. I have now seen some spontaneous imitation. This is pretty remarkable since it has always been very hard to make her imitate anything (and believe me I’ve tried!). One example: As I was putting cutlery on the table before dinner she unprompted took some spoons from the drawer (she is even too short to see what’s in it) and brought them to the table. She has learnt to use two new signs (+20% vocabulary) since day 1 and relearned one sign she previously stopped using.
After 1 month we stopped treatment. First days without medication she was doing strange movements with her hands. Then, slower reactions and not responding as good/fast as before to talking. A lot of staring episodes. Not using signs as much as before. But still happy.
Eventually adverse effects:
-
On day 10 she had a short staring episode when she did not respond to me even when I was yelling her name right beside her. Usually I can see that she is hearing my voice during these events. So I was a little bit shaky thinking immediately at the epilepsy warning on this medication. On the other hand, her staring episodes accelerated without the medicine
Some loose stools at the end of the month.
Spots on the cheeks after food intake; typical histamine reaction, but maybe a bit more of this than before.
/Ling
Ling, very interesting. It does seem that Ponstan should be most effective in very young children, since it is proposed to stop autism getting worse, rather than reverse it. Do you plan to continue?
DeleteThe simple answer is that I would hate being without the effect. As we've restarted Ponstan once again it is obvious that it makes a great impact on language comprehension and imitation skills, and probably on ability to see too. Without it I need to talk so slow word by word and repeat to get her to understand anything.
DeleteBut there are lots of questions that I have unanswered still: Which mode of action is it that makes Ponstan so effective? Is this the best dosage? Why wouldn't Ponstan work for older kids, if it even works for Alzheimer patients? What would be the closest substitute for Ponstan - bumetanide, ibuprofen or something else?
/Ling
Ling, Knut is promoting Ponstan as a means of minimizing the damage caused by the progression of autism. In other words by using Ponstan at an early age you may be able to minimize the severity of future autism. He suggests that early intervention is key, before more damage is done. If it really helps, then keep using it.
DeleteRegarding ponstan
Deletehttp://medcitynews.com/2017/04/q-biomed-early-stage-autism-deal-asdera/?rf=1
http://www.tandfonline.com/doi/abs/10.3109/10715762.2012.669836?src=recsys&journalCode=ifra20
The idea of early intervention is probably true for all interventions, (with the exception of drugs that are not suitable for smaller children). I am looking for a better explanation than that on why Ponstan should work better for toddlers. I just don't want other parents to be discouraged to try it because their kids are 4+ if there isn't a good reason.
DeleteOn the other hand, Bumetanide seems to work best for children around 5 years old according to the scientists themselves, without any obvious explanation. So, which one to choose? Which one works best for say a 3-year old?
Oh, so many questions.
Cheers,
/Ling
Ling, I think the difference between Ponstan and Bumetanide is that Ponstan is suggested to be to some extent disease changing; the idea is you take it for one year, if you are 3 years old. Bumetanide you would need to take for life. Knut has not proved his theory, but I can tell you that Bumetanide is not disease changing; you have to keep taking it.
DeleteIf you look at Knut's papers and patent I think you will find his suggested mode of action.
The UCLA clinician suggested taking both. If you experience no side effects, I think he is likely correct. It is much better to intervene before autism gets worse, which in many children it does after diagnosis.
Peter,
DeleteHave there been instances of disease reversal following mefenamic acid administration in very young kids....say less than three years or its just hypothetical?
Kritika, as Salempeacock highlighted in his link, a company is trying to develop this therapy and is planning a trial.
Deletehttp://medcitynews.com/2017/04/q-biomed-early-stage-autism-deal-asdera/?rf=1
It is hard to prove anything in autism.
Ling is an early adopter, so to speak. There are no published case studies or trials. It is simple and safe. In countries like Greece Ponstan is very widely used as an NSAID in very young children.
Peter, in India too mefenamic acid is widely used in very young children and one can rely on it to bring most fevers down. We used it on my son at the age of one and a half for around ten days when he was hospitalised with typhoid an d still do when he has a fever. Well,it does seem effective in bringing fever down...thats it. Guess we are not as lucky as Ling.
DeleteAs you can see Kritika, I was not able to see any convincable changes until around day 17, and I was definitely looking for it. My daughter was not ill during our trial, something that probably would have spoiled the effect (just like allergy can spoil bumetanide according to Peter). Lastly, my daughter is 2 years old and understands simple directions which make it possible to "measure" reaction time. This would not have been possible at the age of 18 months, when we did not have that two-way interaction.
DeleteThat said, there are of course different ethiologies for autism. In our case I suspect at least one factor is related to calcium and bone marrow.
I don't think Ponstan and bumetanide should be used at the same time (?)
Any ideas btw on how to minimize risks for GI problems with Ponstan?
/Ling
Ling, in the paper from the UCLA doctor:
Deletehttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC4119214/
he suggests first using Ponstan and then later Bumetanide. He is suggesting that Bumetanide may not be wise in very young children. Ben-Ari and Lemmonier do not seem to see any risk in giving bumetanide to very young children.
There is no interaction suggested between Ponstan and Bumetanide.
The GI problems that may occur with Ponstan, or any other NSAID, are often treated by lowering stomach acidity with an H2 blocker (like zantac) or a PPI (like Nexium). In many countries these are OTC. There is lot written about these drugs and autism, look for Dr Timothy Buie at Boston Childrens Hospital. H2 blockers tend to stop working after a time.
Ling, certainly ten days time might not be enough to bring about a perceptible change in behaviour and then an illnesss might further complicate things. About the age factor however, I think I would have still noticed a change at 18 months as I do remember registering a 'fever effect'.
DeleteIn any case, I am not sure, with my son reacting pretty badly to most drugs when given for an extended period how I would have achieved that one year feat of ponstan dosing. Ling, if you do continue with your treatment which fortunately seems effective, do be mindful about the liver....probably a liver friendly diet. I have no idea if ponstan has any hepatic or renal side effects and I am sure you must have checked. Good luck!
Please avoid PPI's. PPI's exist in places you never would have imagined and impair other functions aside from there therapeutic effect. Balance is key. You pay the price for a block or a borrow. When you take medicine that is robbing peter to pay Paul, you will end up with a deficit and cause another problem. Often medicines are not in balance.
DeletePeter, may I ask you for a post on the subject language comprehension and its possible connection to dysfunction in BK, Cav1.3 and KCa2.1-3?
ReplyDelete/Ling
Hi Ling, I'm seeing a new doctor who is very open to using alternative approaches, and I brought up Ponstan. I think he may be open to it, at least for a trial.
DeleteIf you would be so kind, if you've found any success with Ponstan, to share what the impact was, how long it took to see, and what dosage was used? This could be very helpful to making the case to this doctor (I have already sent him the Knut paper) if we knew how long it may take to see an impact and what sort of impact may be seen.
My daughter is 4, and so it seems like Ponstan may be a better option at this point than Bumetanide.
Thanks very much in advance Ling!
AJ
Ok, I was preparing an even longer comment on this, but I do understand the urgency. This is my report:
ReplyDeleteWe decided to make another trial with Ponstan, same dose as described in a comment above. We had again the pleasure to see our daughter imitating, being much more present and understanding (hearing) what we were saying. She even participated in some new imaginative play… There was also some mouthing activities that I had not seen ever before, and for a person with apraxia this is a good sign.
Then, after three weeks I realized that she was wheezing a lot. She did not seem ill, and I found some reports on a rare condition named AERD or Aspirin Induced Asthma. (And we know that rare conditions are not so rare in autism, and that autoimmunity issues are standard.) The very short and maybe not fully correct version of this is that some NSAIDs (COX1 inhibitors) inhibits prostaglandins which upregulates leukotrienes, which may cause “allergy” to NSAIDs. This can manifest itself as urticaria or asthma.
So, we stopped medication for safety reasons. On the very last days with Ponstan my daughter started to say consonants again, and 10 days after the stop she said her first word in 9 months.
----
Ponstan has many effects, probably accessible with different dosages. These I know of:
1. Inhibitor of calcium activated chloride channels
2. Positive allosteric modulator of GABAA receptors (achieved by the above)
3. Stimulating calcium activated potassium channels (at least BK)
4. Anti-inflammatory
5. Analgesic
6. Neuroprotection against β-amyloid induced neurodegeneration
7. Inhibitor of prostaglandins
BK (no. 3) is involved with the electrical tuning of hair cells in the cochlea, so probably that affects language comprehension. I can’t find it now, but I remember a note on “spatial memory” on some other affected ion channel which could relate to the effect of seeing things “not through a pipe”.
----
I can’t say for sure that I recommend trying Ponstan, but I hate every day being without it. Autism is back, but some progressions seems to stay. This is a very clever drug, and I really hope that Knut and the Q-Biomed team can find a workaround before trials.
If your child has problems with receptive language, or does not notice things in his/her surroundings, or you have a history of calcium related illnesses in your family (hypertension, osteoporosis, migraines to mention a few) it would at least be good with a shorter trial to see if these ion channels are a problem in your case. That would tell a lot more than a bumetanide trial. And in the end, maybe there are some workarounds to be found, like a leukotriene antagonist like Montelukast.
Oh, I forgot to mention the 8th effect, see my comment from 15 June.
Delete/Ling
Ling, it looks like about 10% of people with asthma do not tolerate Ponstan. It is listed as a side effect. Many people with autism will develop asthma during childhood. People at risk of asthma often first develop atopic dermatitis. In a study noted in this blog, treating children with atopic dermatitis protected them from developing asthma.
DeleteSo you might conclude from all this that perhaps your daughter has a tendency to develop asthma. If she gets atopic dermatitis you could ask your doctor about ketotifen.
Hi Ling,
DeleteThank you very much for your response! As someone who dealt with asthma symptoms for most of his childhood, I understand how difficult it is.
The information you've provided will really help me make the case for a trial of Ponstan - I hope I can get some improvement if the doc is willing to write the script, and will watch for any atopic dermatitis or breathing issues.
By the way, my "asthma" turned out to be a very strong reaction to certain household chemicals, which triggered a strong asthmatic reaction - laundry detergents, household cleaning solutions, and most powerfully, Bounce dryer sheets, were the cause of my serious symptoms. Ever since I realized the cause, we only use non-scented and natural cleaning products and dryer sheets and I have been asthma free for about 20 years.
Thanks again Ling, it was very kind of you to provide such a detailed response.
AJ
So, I am still on the hunt for something that either would make it possible for us to use mefenamic acid/Ponstan long term (Montelukast?) or would have a similar effect. Does anybody know anything about an asthma drug called Andolast? It should be a mast cell stabilizer and a BKCa-channel agonist.
ReplyDeleteAny other ideas are (desperately) welcome...
/Ling
Ling, Montelukast/Singular is very widely used in childhood asthma as an alternative to steroids. It is cheap.
DeleteIn my son we use a low dose of Flixotide to prevent asthma. This is an inhaled steroid.
There seems to be many flavonoids too that can act as BKCa agonists, at least in vascular ion channels:
DeleteKaempferol, puerarin, dioclein (a flavonoid from the root of Dioclea grandiflora), citrus flavonoid naringenin, quercetin, green tea flavonoids EGCG, and proanthocyanidines, and the nonflavonoid polyphenol resveratrol.
Source: Cardiovascular Ion Channels as a Molecular Target of Flavonoids, 2010
http://onlinelibrary.wiley.com/doi/10.1111/j.1755-5922.2010.00212.x/full
Other ion channels are also mentioned in this paper with corresponding flavonoids, so interesting indeed.
Montelukast has been used in NSAID desensitization protocols, but this path would require an experienced doctor of that field.
Andolast, which is one of the few other drugs that acts as a BKCa opener, just happened to be an asthma drug and mast cell stabilizer, but I don't think it has reached the market yet. It was trialled phase III by Rottapharm, which was then bought by Meda and after that I don't have a clue.
/Ling
I also found a mention on magnolol, a polyphenol derived from Magnolia officinalis, as a BKCa opener.
ReplyDeleteThis extract seems to have numerous interesting properties, though I can't verify that all of them are correct at the time:
-allosteric modulator of GABAa
-anti-oxidative
-anti-inflammatory
-anti-tumorigenic, anti-leukemic
-anti-diabetic
-anti-microbial
-anti-neurodegenerative
-anti-depressant properties
-eventually anti-osteoporotic
-anti-asthmatic
-regulates pain control, hormonal signalling, gastrointestinal and uterus modulation as well as provide cardiovascular and liver protective effects.
-anti NF-kB
-suppress activation of STAT3/JAK pathway
You do wonder if it is too good to be true?
More reading can be found for example here:
http://www.smart-publications.com/articles/relieve-stress-with-honokiol-and-magnolol-from-magnolia-extract
(This is not a paper at all, but does have many references to other, mostly chinese, papers)
/Ling
Ling, there is also Honokiol. I wrote about it and magnolia extract a long time ago. You would have to try them to see if they are potent enough.
DeleteSorry for not doing my homework properly! ;-)
DeleteIt is hard to find something that you haven't written about already.
/Ling
Sorry for posting many comments in a row...
ReplyDelete"Proximal clustering between BK and CaV1.3 channels promotes functional coupling and BK channel activation at low voltage."
https://www.ncbi.nlm.nih.gov/pubmed/28665272
"...revealed striking clusters of CaV1.3 channels surrounding clusters of BK channels and forming a multi-channel complex both in a heterologous system and in rat hippocampal and sympathetic neurons. We propose that this spatial arrangement allows tight tracking between local BK channel activation and the gating of CaV1.3 channels"
And my point is that BK (BKCa) and Cav1.3 are tightly related to each other, and we know since before that both are involved in hearing.
This maybe means that you can choose to either target Cav1.3 or BKCa for language comprehension(??)
/Ling
Ling, Cav1.3 and BKCa are associated with autism, but I do not think you can be sure that a link to hearing loss can extend to language comprehension. I do not think the language problem in autism is caused by a hearing issue. It is more how the data from hearing is processed and where it is processed.
DeleteThere is some interesting research on how children bilingual from birth acquire subsequent languages. It seems to work differently than in monolingual children. We know that bilingual kids can rapidly learn further languages to a high standard. My older son is an example of this.
I think that if your first language develops very late, as in autism, you have missed a developmental window and it gets relegated to the status of a weak second language. Like an American starting learning French in his 20s.
You are right Peter, thanks for letting me know when my theories go a bit haywire.
ReplyDelete/Ling
Anoctamin 2 was identified as an autoimmune target in multiple sclerosis in this paper from 2016:
ReplyDeletehttps://www.ncbi.nlm.nih.gov/pubmed/26862169
"Multiple sclerosis is the most common chronic inflammatory disease of the central nervous system and also is regarded as an autoimmune condition. (..) data revealed prominently increased autoantibody reactivity against the chloride-channel protein anoctamin 2 (ANO2) in MS cases compared with controls. (..) Thus this study represents one of the largest efforts to characterize the autoantibody repertoire within MS."
This raises two questions:
1) Are these autoantibodies also relevant in some cases of autism?
2) If so, is this one of the links from autoimmunity (MIA) to channelopathies?
/Ling
More on the BK channel:
ReplyDelete“In the brain, BK is (..) thought to underlie the fast afterhyperpolarization current and to regulate synaptic transmission by limiting the Ca2+ influx through CaV channels (.. BK channels ..) are activated by the concerted influences of membrane depolarization and increases in calcium concentration. These characteristics explain their proposed role as feedback modulators of the activity of voltage-dependent calcium channels with whom they coexist in both neurons and smooth muscle cells”
http://channelpedia.epfl.ch/ionchannels/209
and
"In the present study, functional roles of a newly identified splice variant in the BK channel α subunit (BKαΔe2) were examined in a human chondrocyte cell line, OUMS-27 (..)
BKαΔe2 knockdown in OUMS-27 chondrocytes increased BK current density and augmented the responsiveness to histamine assayed as cyclooxygenase-2 gene expression. These findings provide significant new evidence that BKαΔe2 can modulate cellular responses to physiological stimuli in human chondrocyte and contribute under pathophysiological conditions, such as osteoarthritis."
https://www.ncbi.nlm.nih.gov/pubmed/27758860
/Ling
It would be interesting to know if Ibudilast and Ponstan/mefenamic acid could be combined. Especially for MS, where these substances seem to have important impacts on myelin and channelopathy respectively.
ReplyDeleteThe two side effects of mefenamic acid to consider are gastric ulcers (long-term use) and aspirin induced asthma.
The latter might be attenuated by Ibudilast since it seems to reduce airway mucus hypersecretion: (https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2010.181.1_MeetingAbstracts.A5620).
Also, the similar PDE4 inhibitor rolipram has been shown to ameliorate aspirin-induced gastric mucosal injury in rats (https://www.ncbi.nlm.nih.gov/pubmed/15986861) and you do wonder if this might be the case with Ibudilast too.
I only found the following text: "The risk or severity of adverse effects can be increased when Ibudilast is combined with Acetylsalicylic acid." So, a question is if this applies to mefenamic acid too and how serious to take this advice.
/Ling
Ling, you could also consider low dose Daxas with Ponstan.
DeleteBeing approved in the EU you check the interactions more easily. Low dose Daxas was found itself not to produce side effects.
https://www.medicines.org.uk/emc/files/pil.5650.pdf
Knut's idea behind Ponstan was to intervene at a very early age (ie now). I think you might want to discuss all this with a well informed doctor, like Agnieszka.
We are on our third round with Ponstan at the moment. And yes, it definitely has the positive effects on language comprehension as before. Or, maybe a little less effect this time... My daughter is older now and maybe I am remembering things differently.
ReplyDeleteWe had to deal with a cold one week and interestingly the effect faded away during this time. To me this is telling us that in our case the positive effect of Ponstan most likely is from it being an positive allosteric modulator of GABA A receptors.
/Ling
Do you believe it would be better to trial low dose Clonazepam or Ponstan first since they both seem to share similar mechanisms?
ReplyDeleteThe mechanisms are not the same. Low dose clonazepam has no side effects, whereas long term use of Ponstan would likely cause GI side effects. You might as well try them both and see if either helps. It depends which is easier to get hold of.
DeleteI was reading literature on tinnitus and found some clues that just maybe can explain the positive experience we’ve had previously with mefenamic acid on language comprehension. It's a hypothesis, so feel free to shoot it down if you think you can.
ReplyDeleteTinnitus is a kind of neural noise, and we all want a better signal to noise ratio especially in the ears as it will affect how much a person can understand from spoken language. My understanding is that tinnitus is closely related to ototoxicity, which is another word for excitotoxicity in the audio regions.
It looks like one way of inducing tinnitus in mice models is to administrate salicylate:
"Large doses of aspirin produce reversible hearing loss and tinnitus. These effects have been attributed to the salicylate ion, the active component of aspirin. [..]
However, the molecular mechanism of salicylate-induced tinnitus remains obscure. [..]
Results showed that the tinnitus induced by salicylate may be suppressed by the introduction of NMDA antagonists into the cochlear fluids."
https://www.ncbi.nlm.nih.gov/pubmed/18225604
Hyperactivity of the NMDA receptors should indeed cause excitotoxicity, and later research has confirmed that this is what happens in tinnitus, whether it is caused by salicylate or high noises.
Further in the above abstract we learn that mefenamate, a salt or ester of mefenamic acid, seems to work in the same way as salicylate:
“we investigated the effect of mefenamate [..] Since NMDA antagonists also blocked mefenamate-induced tinnitus, we suggest that salicylate-induced tinnitus is mediated by [upregulation of] cochlear NMDA receptors through the inhibition of COX activity.”
Now this doesn’t sound good, how could mefenamic acid be beneficial for language comprehension if it causes tinnitus? Again, it is a case of which type of autism you are dealing with. In my child everything points to low-functioning NMDArs being the culprit of many symptoms, so anything that would enhance these (and especially the NR2B and NR2A) subunits) is of great interest.
In an article 11 years later we can see that research has nailed down the ototoxic effect to a specific subunit of the NMDA receptors, the NR2B or GluN2B one:
"Salicylate administration is known to increase GluN2B expression in central auditory regions [in mice]. The present study showed that EGb [Ginkgo Biloba extract] attenuates salicylate-induced GluN2B upregulation in the inferior colliculus [=auditory pathway]."
https://www.e-ceo.org/journal/view.php?number=602
Here we actually get an idea on what to try if the language comprehension is caused by the opposite type of autism with hyperfunctioning NMDArs.
Another NMDAr antagonist, memantine, has been trialled for tinnitus with good results in mice but no beneficial effect in humans. It looks like dosage could be a possible cause here:
"Using the dose adjustment calculation employed by the FDA to calculate human equivalent doses, our dose of 5 mg/kg is approximately equivalent to 56.83 mg/day for a 70 kg human adult. In the only published clinical trial, Figueiredo et al. found no significant effect of 20 mg memantine per day on patients’ tinnitus compared to placebo.
[..]
It is well accepted that although tinnitus can be initiated by noise trauma-induced hair cell damage, once it is established it is generated by hyperactive neurons in the brain. It is possible that at an early stage, blocking NMDA receptors in the cochlea is enough to prevent the further development of tinnitus; once long-term tinnitus has developed, blockade of NMDA receptors in the central nervous system is necessary. Some beneficial effect on tinnitus patients has also been reported with neramexane, which is also an NMDA receptor antagonist"
https://www.frontiersin.org/.../10.../fneur.2012.00127/full
What I haven’t been able to figure out is the missing link to why hypokalemia can induce sound sensory issues (Could it be related to KCNMA1?).
/Ling
Paper showing mefenamic acid has neuroprotective properties in experimental stroke:
ReplyDeletehttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC6374636/
I've read it twice, and though they test a lot of hypothesis' why MFA has this effect, none of them seems to be ther right one.
/Ling
my kid 3,5 year old so do you think ponstan can help. and how much the dose per day for the kid 17kg. plz help me
ReplyDeleteThis is a reply I gave to this same question a short while ago :
DeleteThe pediatric dose for pain/fever for a 2-5 year old is 100 mg 3 times a day.
The adult dose for pain/fever is 500 mg 3 times day.
The original idea patented by Knut Wittkowski to treat very young children with Ponstan was not at a low dose. I do not personally know anyone who gave the high dose to a toddler long term.
Most people giving the low dose of Ponstan long term for autism seem to be using 250mg. Some are adult sized and some are junior school aged.
I would think a logical low dose for a 2 year old would be 50 mg once a day.
The issue with all NSAIDs is their secondary effect as a COX-1 inhibitor; this is what gives the GI side effects. Ponstan is a mild COX-1 inhibitor. At a high dose you would expect to see some side effects, if used long term. At a 1/6 th dose you might never get any side effects. I think this will vary from person to person. You would have to see if any side effects develop, nobody will be able to give a guarantee.
I think you want a low dose that can be given permanently. As the child gets bigger you would have to adjust the dosage gradually to the adult low dose.
You should also note that the ideal time to use an autism therapy is while the child is very young. You stand to gain the most.
ONCE A DAY NOT TWO BRO? I THINK TWO OR THREE IS BETTER BECAUSE HAFL LIFE IS SHORT
DeleteThe point is to avoid the side effects of the standard dose, which limits its long term use.
DeletePeter, do you think use combine bumetanid and ponstan same time is good? my kid used bumex 2 week and seem no effect but i want try more.
ReplyDeleteYou need to try bumetanide for at least a month and at a dosage of 1mg in a young child and 2mg in a teenager. For very young child 0.5mg may be enough.
DeleteIf there is systemic inflammation, this may block the effect of bumetanide. This is why in some people they report that "bumetanide has stopped working". In their child an inflammatory condition has got worse and this raises intracellular chloride and wipes out the effect of bumetanide.
I combine Ponstan with bumetanide. Many people have contacted me to tell me that Ponstan works from them, in both severe autism and adults with Aspergers. I think Ponstan is great - very cheap but highly effective.
Not everyone is going to be a bumetanide responder. For severe autism my guess is at least 30-40%. Which is pretty high for an autism treatment.
i use NAC, Statin and Krill oil with Astanxathin so maybe my kid not imframmatory. Crp and IgA normal
DeletePeter, what you think about that, maybe ALA is better choice
ReplyDeletehttps://journals.plos.org/plosone/article?id=10.1371/journal.pone.0087229
ALA and NAC are both in the thiol class of antioxidant, so their effects are similar, but there are differences.
DeleteFor people with diabetes ALA is usually the best choice.
We used NAC at 1800 to 2400 mg for 10 years, with no side effects at all.
Now that we use Ponstan there is much less need for any NAC at all.
You just have experiment till you find what works best and is well tolerated.
This paper said use long time NAC maybe enhance IL-6 , what you think, i used NAC 6 month . i mean can we find IL-6 by IGE IGM or CRP test?
DeleteYou measure Il-6 with an IL-6 blood test.
Deleteyes, how i know IL 6 enhance or not. get IL 6 blood test.
Delete